Summer 2011, no.8
Menu
Post-eradication – preparing for a lasting polio-free world
The world has seen tremendous gains in polio eradication over the past year. India and Nigeria saw a reduction in cases of almost 95% from 2009 to 2010, and cases of wild poliovirus type 3 (WPV3) fell by 92% globally over the same period. In fact, the last reported case in India had onset of paralysis on 13 January 2011, and India may be on the verge of eradicating polio.
This progress comes just as a study published in Vaccine reports that the economic benefits of eradicating polio would be at least US$40-50 billion, further cementing the case for polio eradication. And while challenges remain, research will continue to play a key role in further evaluating and sensitising strategic approaches to successfully interrupt wild poliovirus transmission globally. Look forward to the next Polio Pipeline, which will focus on operations and communications research.
However, now that the feasibility of polio eradication has been clearly recognized, important questions need to be asked: at what point should the use of oral polio vaccine (OPV) be ceased, and should it be stopped by individual serotype? For example, wild poliovirus type 2 (WPV2) has been eradicated globally since 1999, and since then all type 2 cases are related to the vaccine itself. Is it possible to produce an affordable inactivated polio vaccine (IPV)? How can the risk of vaccine-derived polioviruses be effectively managed immediately after OPV cessation?
These and further questions are the focus of this issue.
Work has already begun on finding the answers. For example, the Strategic Advisory Group of Experts on Immunization (SAGE) IPV Working Group has been working on providing key advice on policy and remaining knowledge gaps. Similarly, the World Health Organization (WHO) and UNICEF have been working with manufacturers to prepare a new agenda to create an adequate stockpile of monovalent oral polio vaccine (mOPV). But there is much more work which needs to be done to prepare for the days when transmission of WPV finally ceases, and research will play a critical role in these plans.
New Roadmap for VDPV Elimination
In 2008, the World Health Assembly (WHA) requested the development of a new strategy to complete the job of polio eradication. The Global Polio Eradication Initiative (GPEI) subsequently developed the new GPEI Strategic Plan 2010-2012. At the start of 2011, epidemiological impact of the new Strategic Plan was already being seen, in particular in some of the world’s most tenacious historic polio reservoirs. And while challenges remain, it is now clear that the interruption of wild poliovirus (WPV) transmission globally is realistically achievable in the near-term. With this feasibility established, efforts must now intensify to prepare for the post-eradication era, in order to meet the overall goal of the GPEI: to ensure that no child will ever again be paralysed by a WPV or a vaccine-derived poliovirus (VDPV).
To this effect, in 2011 the GPEI will produce and develop a new Roadmap for VDPV Elimination. While various strategy and policy documents for post-eradication have been elucidated in the past, including for the eventual cessation of oral polio vaccine (OPV) from routine immunization programmes, this Roadmap will consolidate and supersede all previously-published policy documents. The Roadmap will be regularly updated as new policies are spelled out, and will aim to provide global policy makers at global, regional and country levels an overview of the necessary steps and tools required to fully prepare for the post-eradication era.
At the same time, the Roadmap will clearly outline the humanitarian and economic benefits of a lasting polio-free world (the net benefits of polio eradication having been estimated at US$40-50 billion), and as such will provide the international donor community with justification for continued investment into the GPEI for the post-eradication era, to facilitate long-term planning and budgeting processes.
The new Roadmap will consolidate all previously-published policy documents, including the “OPV Cessation Framework” published in 2005
A lasting polio-free world
Ensuring no child will ever again be paralysed by a wild – or vaccine derived polio virus.
OPV cessation – time to proceed by individual serotypes?
Discussions are ongoing to ″kick–start″ the process by removing serotype 2 components from existing routine immunization vaccines.iince 1999 (when wild poliovirus type 2 – WPV2 – was eradicated globally), increasing scientific data demonstrate that polio eradication will also require the eventual cessation of oral polio vaccine (OPV) in routine immunization programmes. Otherwise, the continued reintroduction of the attenuated polioviruses of OPV into a polio-free world will result in polio cases due to vaccine-associated paralytic polio (VAPP), and polio outbreaks due to circulating vaccine-derived polioviruses (cVDPVs).VAPP cases are extremely rare. The total VAPP risk is approximately 2-4 per one million birth cohort. VAPP results from small genetic mutations which the live vaccine-virus undergoes when replicating in the human gut (ie which make the virus ‘revert’ to being neurovirulent). Children with immuno deficiencies tend to be at substantially higher risk of developing VAPP after immunization. Based on current usage of trivalent OPV around the world, between 250 and 500 VAPP cases occur annually.Equally rare, the attenuated OPV viruses can – over time – genetically change from the original strain contained in OPV to become a cVDPV, effectively regaining both the ability to cause paralysis in humans, and to circulate, similar to wild polioviruses (WPVs). Worldwideover the past ten years, over 10 billion doses of OPV have been administered to more than 2.5 billion children, and as a result more than 3.5 millionpolio cases were prevented. During that time, 18 outbreaks of cVDPV shave occurred, in 16 countries resulting in 510 VDPV cases.It has long been understood that the small risk of VAPP and VDPVs paled in significance to the tremendous public health benefits associated with OPV, particularly when WPV transmission was widespread. Every year, hundreds of thousands of cases due toWPV are prevented. Well over eight million cases have been averted since large–scale administration of OPV began twenty years ago. But it has also been long understood that there would come a time when the balance of benefit versus risk of trivalent OPV would begin to tip. In other words, when the only cases of polio occurring are due to VAPP or cVDPVs, and the risk of WPV cases occurring has been virtually eliminated (in many countries of the world which have already interrupted WPV transmission, the use of OPV has already been stopped due to this risk, and replaced with routine immunization with IPV). On a global level, that balance would be right around the time of global interruption of WPV transmission.That is why the cornerstone strategy for the post–eradication era is to eliminate the risk posed by OPVs by eventually stopping the use of all live oral polio vaccines, for routine and supplementary immunization, as soon as possible after the eradication of WPVs.OPV cessation, it has been foreseen, would occur as soon as possible after the last case
of WPV has been detected globally. At a time when immunity levels remain relatively high and disease surveillance sensitive. But with the large proportion of VAPP cases caused by the type 2 serotype contained in trivalent OPV, and WPV2 transmission having already been successfully interrupted (since 1999), calls are becoming louder to remove all type 2-containing OPV at this time already.
The call makes sense from a public health point of view, especially since the availability of the new bivalent OPV (introduced in late 2009), containing only type 1 and type 3 serotypes (the only two WPV serotypes remaining in circulation). It would essentially mean that bivalent OPV would replace trivalent OPV across the board, in routine immunization programmes.
Based on current OPV usage, between 250 and 500 VAPP cases occur every year, a large proportion due to the type 2 component in trivalent OPV.©WHO
In other words, to stop using type-2 oral vaccine virus even before the remaining strains of WPV1 and WPV3 transmission have been globally interrupted.The discussions, led first and foremost by the Strategic Advisory Group of Experts on Immunization(SAGE) and its subsidiary body the SAGE IPV Working Group(established to advise SAGE on pre– and post–eradication polio vaccination policy), is a recognition that theexpected shift in balance from benefit to risk-for type 2-containing OPV-has indeed already occurred. But is a global OPV type 2 cessation effort, at this time – even before WPV eradication – operationally feasible?
OPV type 2 cessation: bivalent OPV would replace trivalent OPV accross the board
The primary risk associated with OPV type 2 cessation would be the rapid increase in susceptible populations to poliovirus type 2. This in turn would increase the risk of new type 2 cVDPVs emerging, in the immediate interim period following OPV type 2 cessation. Equally important would be the rapid stopping of any eventual residual type 2 cVDPVs, ongoing from just immediately prior to OPV type 2 cessation. To safely implement an OPV type 2 cessation programme would therefore require the implementation of a number of strategies to manage these risks.
In the first instance, the formal validation of the global interruption of WPV2 transmission will need to occur, due of the ongoing risk of poliovirus importations into polio-free areas. This will be particularly important in the three Regions which remain endemic to WPV1 and WPV3 transmission (Africa, the Eastern Mediterranean and South-East Asia).Highly sensitive surveillance for all polioviruses, including type 2 wild and vaccine-derived polioviruses will need to be maintained, both to document the elimination of type 2 poliovirus transmission (including residual type 2 cVDPVs), and torapidly detect the potential re-introduction or reemergence of any type 2 poliovirus (WPV or cVDPV). Atthe same time, outbreak response capacity will have to be maintained, including ensuring thesupply and management of stockpiles of appropriate type 2-containing vaccines to facilitate and Sabin typeappropriate outbreak response should it be necessary.All WPV2 and Sabin type 2 viruses must be placed under appropriate biocontainment levels on a timely basis to minimise the risk of re-introduction into a type 2 polio- free world.
Adequate supplies of bivalent OPV and IPV will need to be secured. IPV will be needed for countries that elect to retain type 2 poliovirus in laboratories, for countries that produce IPV, and for countries choosing to introduce IPV as a risk mitigation strategy, particularly to maintain type 2 population immunity and thereby reduce the consequences of apotential re-introduction or reemergence of type 2 polio.
And finally, the cessation of OPV type 2 will need to be synchronized, either globally or regionally, to ensure that no country is inadvertently put at risk of importing a type 2 cVDPV from a country that continues to use type 2 containing OPV.
Preparing for OPV type 2 cessation
Managing the risks by:
Validating global interruption of WPV2 transmission
Maintaining sensitive surveillance and outbreak response capacity
Appropriately containing all type 2 polioviruses
Ensuring supplies of bivalent OPV, and affordable IPV
Synchronizing OPV type 2 cessation globally/ regionally
If properly implemented, OPV type 2 cessation would have significant public health benefits. Over the past ten years, more than 80% of all cVDPV cases were due to type 2. Of the estimated 250-500 annual VAPP cases, up to 38% are due to to type 2. These case numbers would no longer occur. In addition to these significant humanitarian benefits, OPV type 2 cessation would provide the GPEI with a ‘push’ for global OPV cessation of all oral polio vaccines. Feasibility of OPV cessation would be underscored in practice, and would ensure a ‘trial run’ for all OPV cessation. Key lessons would be learnt to ensure that this process can be implemented in the safest and most efficient manner.
Significant benefits of OPV type 2 cessation Up to 200 VAPP cases prevented
every year Up to 80% fewer cVDPV events Feasibility of OPV cessation translated into practice,providing key lessons for all OPV cessation.For these reasons, the SAGE IPV Working Group at its April 2011 meeting concluded that it would be appropriate to consider planning for the cessation of routine OPVimmunization against type 2 polioviruses. Research will continue to play a key role in preparing for both the eventual cessation of all OPVs and the potential cessation of type 2 OPV. Policy bodies, including an Expert Consultation on VDPVs and the next SAGE meeting, both in November 2011, and the Executive Board of WHO in January 2012 are expected to review further arguments. But it is entirely feasible that come this time next year, the GPEI will be in the midst of a OPV type 2 cessation programme, as it continues on its final stretch to rapidly interrupt the remaining chains of WPV1 and WPV3 transmission globally. Public health and programmatic arguments certainly would speak favourably for such an approach.
lasting polio-free world.
I safely managing the transition period following cessation of oral polio vaccine (OPV) from routine immunization programmes (ie the period between OPV cessation and the elimination of any residual vaccine-derived polioviruses – VDPVs) will be key to securing a lasting polio-free world. This will require in the first instance the ability for countries to maintain population immunity against polio. Following OPV cessation, inactivated polio vaccine (IPV) will be the only option with which to do so.
Recognizing that current costs of IPV are substantially higher than OPV, the Global Polio Eradication Initiative (GPEI) has intensified its programme of work to study a range of affordable IPV strategies. The four branches of this work are: schedule reduction (evaluating the use of one or two IPV doses to immunize and/or prime children); dose reduction (evaluating fractional dose IPV given intra-dermally by needle-free device or micro-needle patch to spare antigen); antigen reduction (using adjuvant to reduce antigen contents per dose); and, production cost reduction (further optimizing production processes and producing IPV in developing countries with less or non-infectious strains). the dates of conclusions of the bilateral agreement with RIVM. WHO and RIVM will continue the
An animal study completed in 2010 suggested that a ten-fold reduction of IPV antigen is feasible with inclusion
In collaboration with the Netherlands Vaccine Institute (NVI), and more recently the National Institute for Public Health and the Environment (RIVM) in the Netherlands, clinical lots of seed-strains of IPV produced from Sabin poliovirus have been prepared. Traditional IPV is manufactured using wild poliovirus and an inadvertent biocontainment failure could be associated with serious consequences in some areas of the world in the post-eradication era (ie areas with high population density, inadequate sanitation infrastructure and low population immunity levels). Sabin seed strains for IPV have the advantage over wild polioviruses that they are attenuated, and hence are safer for handling and IPV production in developing country settings in the posteradication era.
In this first phase of a broader intended technology transfer programme, this new technology will be transferred to two manufacturers for vaccine production: Panacea Biotech, Ltd in India, and LG Life Sciences, Ltd in the Republic of Korea. Both manufacturers have confirmed their intention to use all reasonable efforts to apply for registration of their Sabin IPV products in the country of production within four years from technology transfer programme this year with further manufacturers.
In addition, six research collaborations are ongoing to assess further attenuated poliovirus strains, including with the University of California at San Francisco, the US Centers for Disease Control and Prevention (CDC), the National Institute for Biological Standards and Control (NIBSC) in the United Kingdom, the University of Leeds, and two projects with State University of New York (SUNY).
The other option to address risks of VDPVs is treatment with antiviral drugs. Dozens of antiviral compounds have been tested for activity against polioviruses, with two promising candidates now in clinical developmentManaging transition period after OPV cessation. Such antivirals could play a key role in ensuring that infections are rapidly cleared in immunodeficient individuals who might be chronically shedding poliovirus. At the same time, antivirals could offer protection for persons exposed to poliovirus (eg through unintentional laboratory exposure) and for communities exposed to cVDPVs.
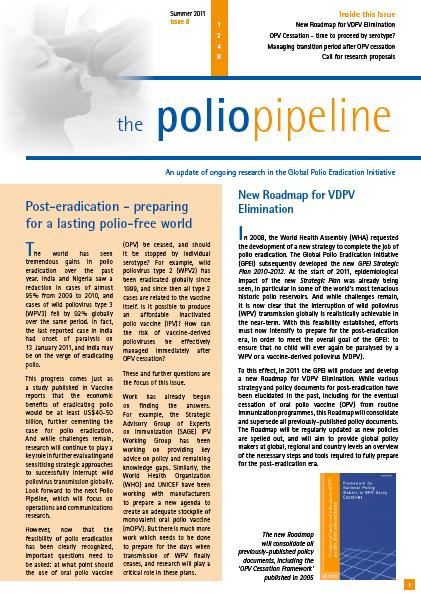
Finally, progress continues to be made in developing an OPV stockpile to respond to residual cVDPVs. By the end of 2010, nine monovalent OPVs (for type 1 and type 3 polio) had been licensed, and a global stockpile is under tender. The global stockpile of monovalent OPVs, and internationally-agreed processes for its management and use, will be critical to carry out timely response to any residual cVDPVs in the post-eradication era.
New knowledge will help further elucidate post-eradication strategies
ioutine and supplemental immunization activities using live (attenuated), Sabin-vaccine strains are the best strategy to eradicate polio but can also lead to circulation of Sabin- Like (SL) viruses, and consequently to vaccine-derived polioviruses (VDPVs) that are related to vaccine strains but with significant genetic changes. The latter are of programmatic interest as they can gain ability to provoke acute flaccid paralysis (AFP) in infected people. Detecting these viruses can be also challenging due to both genetic and antigenic changes.
Since 2007, and as part of the continuous monitoring and improvement of poliovirus diagnostics, the global specialized polio laboratory at the US Centers for Disease Control and Prevention (CDC) has made great efforts to set up rapid and reliable methods to detect VDPVs, including the ones that have gained the capacity to be transmitted from person-to-person. The outcome is two validated new methods, using real-time reverse transcriptase polymerase chain reaction (rRT-PCR), to say if the polioviruses isolated from stool samples are wild or Sabin-like and, in a second step, if the latter are VDPV or not. Importantly, these new procedures have also reduced the average time needed to confirm poliovirus by 50% (from 42 days to 21 days).
Consequently, in 2009, the Global Polio Laboratory Network (GPLN) has started to implement a validated new testing algorithm using both methods. Additional data gathered since then clearly show that this new algorithm is faster and more reliable for the detection of both wild polioviruses and VDPVs. Then, further genetic characterization of suspected VDPVs by sequencing, along with clinical and epidemiological data, allow the classification as (i) circulating VDPVs or (ii) immunodeficiency-associated VDPVs (iVDPVs). Notification of these VDPVs by the GPLN during past years has considerably increased knowledge on prevalence, geographical location and key virological and clinical features of these viruses.The implementation of rRT-PCR procedures was significantly expanded in 2010, and has played a critical part in further enhancing detection of all polioviruses, to enable rapid outbreak response. Data gathered since the implementation of this new algorithm since 2009 will be reviewed in late 2011 during an extended consultation on VDPVs,
to further sensitise strategies for early detection, reporting and response to VDPV emergences. These strategies will be critical for the post-eradication era. Overview of WHO-supported research on iVDPVs and outcomes to date
The Global Polio Eradication Initiative (GPEI) has committed to supporting a series of studies in up to ten middle and low-income oral polio vaccine (OPV)-using countries to generate information regarding the prevalence of long-term poliovirus excretion among persons with primary immune deficiencies (PIDs). It has been confirmed that persons with prolonged poliovirus excretion, such as can be the case with those suffering from PIDs, could theoretically transmit virus to contacts and the general population following interruption of wild poliovirus transmission. These polioviruses are called immunodeficiency-associated vaccinederived polioviruses (iVDPVs), suggesting these viruses have replicated and evolved in immuno-compromised individuals. The objectives of this study series are to: 1) estimate the prevalence of vaccinederived poliovirus (VDPV) excretion among persons diagnosed with primary immune (B-cell or combined B/T-cell) deficiency disorders; 2) genetically characterize VDPVs isolated from persons with PIDs; and 3) follow-up/monitor study subjects who have tested positive for VDPV excretion to determine duration of excretion.This information is essential to understanding the future risk of VDPV circulation, development of effective immunization policies, and ultimately polio eradication. Whereas the risk of circulating VDPVs (cVDPVs) will likely be time-limited following OPV cessation, the risk of reintroduction of VDPVs by persons with PIDs may persist as long as there are persons excreting iVDPVs. The successful surveillance of these viruses will therefore take on an increasing importance and it has been suggested that this study series could serve as a roadmap for the development of national surveillance systems to detect and respond to iVDPVs. A pilot effort for such a surveillance system has been implemented in Egypt as part of the work associated with this study series.
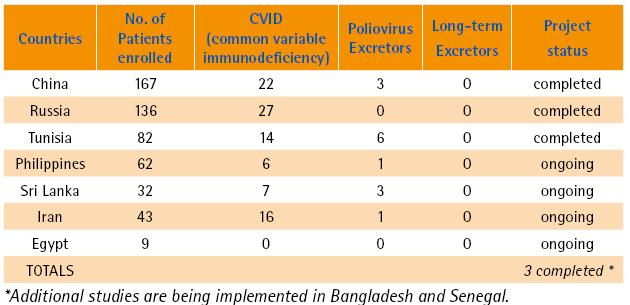
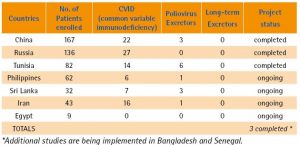
In April 2011, the World Health Organization (WHO) hosted a meeting of study investigators and other relevant experts in order to review progress and results to date among the different iVDPV Prevalence Studies and the Egypt iVDPV Surveillance Project. The meeting agenda included a discussion of the possible application of polio antivirals for the treatment of chronic poliovirus excretors. Some preliminary results of countries in which enrolment and data collection exceeds six months appear in the following table. These results illustrate in particular that the incidence of excretors is low and no long-term excretors have been identified to date in any of the studies.In all studies, excretors have been sought out through both the testing of known or suspected persons with PIDs or through the investigation of acute flaccid paralysis (AFP) cases. Only very few of the participating countries have established registries of persons with PIDs. Based on experience to date, AFP surveillance appears to be the most effective form of detection of iVDPVs. Having a treatment to be recorded to add value to the offer patients could facilitate surveillance efforts. A total of 531 patients have been enrolled to date in the country study sites which reported results at this meeting. 14 (2.6%) of these were found to excrete poliovirus (as per the results table above). However, none so far have proven to be long-term (> 6 months) excretors. 92 out of those 531 (17%) enrolled patients suffered from common variable immunodeficiency (CVID), suggesting that the upper 95% confidence bounds associated with a chronic excretor within this group remains substantially above zero. Among the key data this study series can offer are the upper bounds of how many cases can be typically expected from a given population, but it was noted that additional data could study results. The benefits of these studies could be maximized as follows:
1) For Polio Eradication: Better defining the risks associated with iVDPVs and providing a model for the eventual integration of this work into routine surveillance. 2) For Patients with PIDs: Preventing a new generation of excretors and identifying potential recipients of antiviral treatment.
Overview of WHO-supported research on iVDPVs and outcomes to date
ihe Global Polio Eradication Initiative (GPEI) has committed to supporting a series of studies in up to ten middle and low-income oral polio vaccine (OPV)-using countries to generate information regarding the prevalence of long-term poliovirus excretion among persons with primary immune deficiencies (PIDs). It has been confirmed that persons with prolonged poliovirus excretion, such as can be the case with those suffering from PIDs, could theoretically transmit virus to contacts and the general population following interruption of wild poliovirus transmission. These polioviruses are called immunodeficiency-associated vaccinederived polioviruses (iVDPVs), suggesting these viruses have replicated and evolved in immuno-compromised individuals. The objectives of this study series are to: 1) estimate the prevalence of vaccinederived poliovirus (VDPV) excretion among persons diagnosed with primary immune (B-cell or combined B/T-cell) deficiency disorders; 2) genetically characterize VDPVs isolated from persons with PIDs; and 3) follow-up/monitor study subjects who have tested positive for VDPV excretion to determine duration of excretion. This information is essential to understanding the future risk of VDPV circulation, development of effective immunization policies, and ultimately polio eradication. Whereas the risk of circulating VDPVs (cVDPVs) will likely be time-limited following OPV cessation, the risk of reintroduction of VDPVs by persons with PIDs may persist as long as there are persons excreting iVDPVs. The successful surveillance of these viruses will therefore take on an increasing importance and it has been
suggested that this study series could serve as a roadmap for the development of national surveillance systems to detect and respond to iVDPVs. A pilot effort for such a surveillance system has been implemented in Egypt as part of the work associated with this study series. In April 2011, the World Health Organization (WHO) hosted a meeting of study investigators and other relevant experts in order to review progress and results to date among the different iVDPV Prevalence Studies and the Egypt iVDPV Surveillance Project. The meeting agenda included a discussion of the possible application of polio antivirals for the treatment of chronic poliovirus excretors. Some preliminary results of countries in which enrolment and data collection exceeds six months appear in the following table. These results illustrate in particular that the incidence of excretors is low and no long-term excretors have been identified to date in any of the studies.
surveillance appears to be the most effective form of detection of iVDPVs. Having a treatment to be recorded to add value to the offer patients could facilitate surveillance efforts.
A total of 531 patients have been enrolled to date in the country study sites which reported results at this meeting. 14 (2.6%) of these were found to excrete poliovirus (as per the results table above). However, none so far have proven to be long-term (> 6 months) excretors. 92 out of those 531 (17%) enrolled patients suffered from common variable immunodeficiency (CVID), suggesting that the upper 95% confidence bounds associated with a chronic excretor within this group remains substantially above zero. Among the key data this study series can offer are the upper bounds of how many cases can be typically expected from a given population, but it was noted that additional data could study results. The benefits of these studies could be maximized as follows:
In all studies, excretors have been sought out through both the testing of known or suspected persons with PIDs or through the investigation of acute flaccid paralysis (AFP) cases. Only very few of the participating countries have established registries of persons with PIDs. Based on experience to date, AFP
1) For Polio Eradication: Better defining the risks associated with iVDPVs and providing a model for the eventual integration of this work into routine surveillance.
2) For Patients with PIDs: Preventing a new generation of excretors and identifying potential recipients of antiviral treatment.
The Polio Research Committee (PRC) is currently soliciting research proposals to support the implementation and evaluation of the Global Polio Eradication Initiative (GPEI) Strategic Plan 2010-2012, with particular focus on the following topics.
1. Operational research
A key aspect of the GPEI Strategic Plan 2010-2012 is to continuously review the quality of surveillance for supplementary immunization activities (SIAs) and fill critical gaps in quality. The GPEI is interested in research proposals to aid the process of identification of high-risk areas, support and facilitate evidence-based solutions to improve programme immunization operations.
Operational research priorities to be considered for funding include:
1. Identification of key issues in areas with persistent polio transmission and/ or repeated importations resulting in re-established transmission;
2. Social research to understand migratory populations and implications to the polio epidemiology in polio-infected countries (e.g., the size and pattern of migration and their knowledge, attitude and practice towards immunization and general healthcare seeking behaviour);
3. Evaluation of alternative operation model for the quality coverage of migratory populations during SIAs; and,
4. Evaluation of initiatives to improve operations in areas with compromised security (e.g., short interval additional doses, alternative operational model to address security risks).
2. Communication research
The Independent Monitoring Board (IMB) report released in April 2011 recommended that the GPEI address complex operational or interpersonal difficulties in local communities (“worm’s eye view” of realities on the ground). Accordingly, the GPEI is soliciting proposals in the area of communication research, which help identify and address challenges and monitor performance in polio communication.
Some potential communications
research subjects include:
Evaluation of risk perception and risk communication among vaccine recipients and health workers;
Innovative survey approaches to generate social data which does not rely on selfreported process indicators;
Analysis of non-compliance and anti-vaccine behaviour (e.g., rumour surveillance) in order to develop better designed and more appropriately targeted interventions; and,
Evaluation of different communication interventions to promote knowledge, behaviour change and improve acceptance, including improved documentation of both successes and challenges concerning the demand for polio vaccine.
3. Evaluation of improving and utilizing IPV
The ability to affordably maintain immunity against polio in countries which choose to do so will be key to safely managing the transition period following OPV cessation, after which inactivated polio vaccine (IPV) will be the only appropriate polio vaccine.
Preparing for the wider use of IPV, the GPEI has intensified its programme of work to study a range of affordable IPV strategies and assess the feasibility and effectiveness of IPV introduction.
Especially, the following focus are of interest:
1. Evaluation of immunological mechanisms and persistence of priming among infants vaccinated with IPV;
2. Assessment of impact of adding IPV on SIA quality (e.g., coverage); and,
3. Assessment of VDPV emergence after the switch from OPV to IPV-only schedule in national immunization programme in developing countries.
4. Improving routine immunization activities with GPEI infrastructure
Ensuring strong immunization systems for the delivery of routine childhood vaccines has been one of the four core strategies of the GPEI since its launch in 1988. The GPEI is interested in a pilot project to utilize GPEI assets (e.g., skilled
human resource, immunization infrastructure, operating know-how) to improve the quality of routine immunization.
5. Improving acute flaccid paralysis (AFP) surveillance
Surveillance for cases of acute flaccid paralysis (AFP) is the core strategy employed by the GPEI to detect the transmission of wild polioviruses or circulating vaccinederived polioviruses, guide SIA strategy, and facilitate the eventual certification of eradication. In some areas of the world, there are still surveillance gaps in key highrisk areas. The GPEI is interested in a pilot project to address these known gaps through the use of new technology (e.g., geographic information system – GIS, or short message service – SMS).
Research proposals are invited from GPEI staff (e.g., EPI managers) and independent institutions/investigators, as well as private cooperations.
Procedure for submission of proposals:
All research proposals should include the following information:
Research question/ objectives (e.g., research questions, reference to published literature and cutting-edge science, description of how the results will be utilized).
Qualification of investigators and collaborators (e.g., track record of researchers, capability of laboratory, necessary contractual arrangements).
Budget request (e.g., appropriate for work anticipated).</p
Study design and methodology (e.g., detailed activities, timelines, deliverables, availability of necessary capacities, feasibility of methods, plans for ethical and government approvals).
The standard research proposal form is available here.
Researchers are invited to submit proposals by 31 July 2011 to the:
Research and Product Development team
Global Polio Eradication Initiative, WHO, Geneva,
by email to
polioresearchATwho.int.
- Progress report by the GPEI Secretariat to the 64th World Health Assembly, 16-24 May 2011, Geneva, Switzerland.
- Reports of the 2nd and 3rd meetings of the Independent Monitoring Board.
- GPEI Financial Resource Requirements (FRR) – July update.
- 2011 edition of WHO’s International travel and health vaccination recommendations for travellers. April 2011.
- Meeting of the Strategic Advisory Group of Experts on immunization: conclusions and recommendations. Weekly Epidemiological Record. 20 May 2011, vol 86, 21 (pp 205-220).
- Progress towards interrupting wild poliovirus transmission worldwide: January 2010 – March 2011. Weekly Epidemiological Record. 13 May 2011, vol 86, 20 (pp189-204).
- Monitoring progress towards global polio eradication: poliovirus surveillance, 2009- 2010. Weekly Epidemiological Record. 15 April 2011, vol 86, 16 (pp 153-160).
- Outbreak of poliomyelitis, Republic of the Congo, September 2010-February 2011. Weekly Epidemiological Record. 8 April 2011, vol 86, 15 (pp 141-152).
- Performance of acute flaccid paralysis (AFP) surveillance and incidence of poliomyelitis, 2010. Weekly Epidemiological Record. 1 April 2011, vol 86, 14 (pp 129-140).
- Bakker WAM, Thomassen YE, van der Pol LA (2010). Scale-down approach for animal-free polio vaccine production. In: Noll Th, ed., Cells and Culture; Proceedings of the 20th ESACT meeting, June 17-20, 2007, Dresden, Germany. Springer, Dordrecht, 4(6):541– 550
- Thomassen YE, van Sprang ENM, van der Pol LA, Bakker WAM (2010). Multivariate data analysis on historical IPV production data for better process understanding and future improvements. Biotechnol. Bioeng. 107(1):96–104
- Westdijk J, Brugmans D, Martin J, van ’t Oever A, Bakker WAM, Levels L, Kersten G (2011). Characterization and Standardization of Sabin based Inactivated Polio Vaccine. Proposal for a new antigen unit for inactivated polio vaccines. Vaccine 29(18):3390–3397
- Verdijk P, Rots NY, Bakker WAM (2011). Clinical development of a novel inactivated poliomyelitis vaccine based on attenuated Sabin poliovirus strains. Expert Review of Vaccines. 2011; 10:635-644
- John TJ, et al. Monovalent type 1 oral poliovirus vaccine among infants in India: Report of two randomized double-blind controlled trials. Vaccine, 2011, doi:10.1016/j. vaccine.2011.04.133 in press
Meeting |
Date |
Venue |
| International Workshop on Polio Eradication: Securing the gains – cross-regional collaboration in protecting polio-free areas | 21-22 July 2011 | Urumqi, Xinjiang, China |
| WHO Regional Committee for Africa | 29 August – 2 September 2011 | Abidjan, Côte d’Ivoire |
| WHO Regional Committee for South-East Asia | 6-9 September 2011 | Jaipur, India |
| WHO Regional Committee for Europe | 12-15 September 2011 | Baku, Azerbaijan |
| Polio Research Committee (PRC) | 17-18 September 2011 | Sapporo, Japan |
| WHO Regional Committee for the Americas | 26-30 September 2011 | Washington DC, USA |
| 17th Informal Consultation of the Global Polio Laboratory Network | 27-28 September 2011 | Geneva, Switzerland |
| WHO Regional Committee for the Eastern Mediterranean | 2-5 October 2011 | Cairo, Egypt |
| WHO Regional Committee for the Western Pacific | 10-14 October 2011 | Manila, Philippines |
| Expert Consultation on VDPVs | November 2011 | Geneva, Switzerland |